2. What is Type 2 Diabetes
Diabetes happens when the body cannot make insulin, or when the insulin does not work properly.
There are different types of diabetes, and the treatment can be different depending on the type:
Type 1 diabetes - the body stops making insulin
Type 2 diabetes - the body still makes some insulin but it doesn't work well
Steroid or medication induced diabetes - some medicines can cause high blood sugar, which may lead to diabetes
What is insulin?
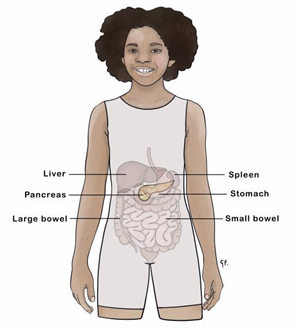
Insulin is a hormone made by the pancreas, which is a small organ behind the stomach. When we eat food, it's broken down in the stomach and gut. Foods with carbohydrates (like bread, rice, fruit and sugar) turn into glucose (a type of sugar), which goes into the bloodstream.
Insulin helps move the glucose from the blood into the body's cells, where it is used for energy. Without insulin, glucose can't get into the cells, so the body doesn't get the energy it needs to work properly.
What is Type 2 diabetes?
Type 2 diabetes happens when the body doesn't use insulin properly. The pancreas still makes insulin, but the body's cells don't respond to it well or use it properly - this is called insulin resistance. Because of this, the body needs more insulin to do the same job. Over time, the pancreas can get tired and may not make enough insulin.
Insulin helps move glucose (sugar) from the blood into the body's cells to be used for energy. When there isn't enough insulin, or it's not working properly, glucose stays in the blood, causing high blood sugar levels.
Type 2 diabetes is more common in adults, but some children and young people can get it too.
The good news is that Type 2 diabetes can sometimes be prevented or delayed by making healthy lifestyle changes.
👉 You can watch a helpful video from Kidshealth that explains this more: https://kidshealth.org/en/teens/type2.html
What are the signs of Type 2 diabetes?
When blood glucose levels are too high, it can cause symptoms like:
feeling tired or having low energy
blurry vision
feeling very thirsty
needing to pee more often or waking overnight to pee
weight loss
feeling sick
trouble paying attention at school or finding it hard to get up for school
mood changes
getting infections often or cuts that take longer to heal
One of the first signs in children can be dark patches of skin in places like the neck, armpits, behind the knees or groin. This is called Acanthosis Nigricans and is a sign that the body isn't using insulin well.

In tamariki and rangatahi, Type 2 diabetes can develop more quickly and be more aggressive than in adults. That's why it is so important to have regular checkups and to work alongside the diabetes team to help manage the condition early and prevent long-term health problems.
| 📌 Important to Know Sometimes, Type 2 diabetes develops slowly and there might be no clear symptoms. In some cases, it’s only picked up during a routine blood test. |
Who is more likely to get Type 2 diabetes?
Some tamariki and rangatahi have a higher chance of getting Type 2 diabetes, especially if they have more than one of these risk factors:
a family history of diabetes (like grandparents, parents, brothers or sisters)
are of Māori, Pasifika, Asian or Middle Eastern descent
being overweight
not being very active ( less than 60 minutes of exercise or activity most days)
Treatment of Type 2 diabetes
Healthy lifestyle changes
The best support for tamariki and rangatahi living with Type 2 diabetes is focusing on healthy lifestyle changes - including nourishing kai (food) and increasing movement and activity.
These changes can really help their health and help the body use insulin better.
Changing habits can be hard, but when whānau come together with aroha and support each other, it gets easier. Starting with small changes is often better than trying to do everything at once.
Your diabetes team can help you and your whānau make a plan with simple, clear goals that work for you.
Want to know more about healthy lifestyle changes?
Information on food choices: https://www.kidshealth.org.nz/diabetes/type-2-diabetes-in-children-general-guidelines-on-nutritional-management
Information on exercise : https://www.kidshealth.org.nz/diabetes/encouraging-children-young-people-with-diabetes-to-be-active
For healthy meal ideas and recipes, look for these websites:
On the Internet, look for these websites:
Tablets
Metformin tablets
Metformin is a medicine that helps the body use insulin better.
Some tamariki and rangatahi will need to take Metformin tablets once or twice a day. Your diabetes team will talk with you about a plan if Metformin is needed.
Metformin works best when taken regularly. It can help to take the tablet at the same time as kai (food) to remember. Parents, caregivers should always supervise that the tablets have been taken and help make sure the medicine is taken safely.
If your tamaiti is vomiting or unwell, or needs certain scans like a CT scan, Metformin should be stopped during that time and started again once they are better.
It's also best to avoid alcohol while taking Metformin.
For more information you can download and read the leaflet in this link
Empagliflozin
This is a medicine that helps lower blood sugar levels. It comes in two forms:
Jardiance (Empagliflozin on its own): This helps the body get rid of extra sugar by passing it out in the urine. It also has extra health benefits — it can help protect the heart and kidneys, which is especially helpful for people with diabetes.
Jardiamet (Empagliflozin + Metformin): This is a mix of two medicines in one tablet. It works in two ways:
Empagliflozin removes extra sugar through the urine.
Metformin helps the body use insulin better.
Together, they help lower blood sugar and support long-term health.
These medicines need to be taken every day to work properly.
See a helpful video: https://youtu.be/s7Zz16ucCow
A patient leaflet on Empagliflozin can be downloaded here.
Injections or shots
GLP-1 Medicines (like Victoza and Trulicity)
GLP-1 medicines are a newer type of treatment for Type 2 diabetes. They help the body release insulin when blood sugar is high, slow down how quickly food leaves the stomach, and reduce appetite. This helps lower blood sugar levels and can also support healthy weight loss.
One of the great benefits of GLP-1 medicines is that they can help with weight management by reducing hunger and helping tamariki and rangatahi feel full for longer. This can make it easier to eat less, make healthier food choices, and work towards a healthier weight—an important part of managing Type 2 diabetes.
GLP-1 medicines may also help protect the heart and kidneys, which are important to care for when living with diabetes.
Some tamariki may have side effects like feeling sick (nausea), upset stomach, or diarrhoea—especially at the beginning. These usually settle over time. Eating smaller meals and starting at a low dose that increases slowly can help reduce side effects. If your tamaiti has side effects, it’s best not to stop the medicine on your own—talk with the diabetes team. They can adjust the dose or suggest ways to manage any discomfort.
Victoza (Liraglutide)
Victoza is given as a once-daily injection under the skin using a simple pen device. It helps lower blood sugar and reduce appetite, which can support steady and healthy weight loss over time. Because it's taken daily, your diabetes team can closely adjust the dose to suit your tamaiti's needs.
Want to know more about this medicine?
Victoza (liraglutide) factsheet Healthify He Puna Waiora, NZ, 2023, in the following languages:
See also tips on starting GLP-1
Trulicity (Dulaglutide)
Trulicity works similarly to Victoza but is only taken once a week, which can be more convenient for busy whānau or rangatahi who prefer fewer injections. It also comes in an easy-to-use pen that’s ready to go—no mixing or preparation needed.
Want to know more about this medicine?
See https://trulicity.lilly.com/how-to-use
See also information to download or read on trulicity
Insulin injections
For some tamariki and rangatahi with Type 2 diabetes, their bodies can’t make enough insulin on their own. Without enough insulin, sugar builds up in the blood, which can make your tamaiti feel unwell and cause problems over time.
When this happens, insulin injections may be needed to help keep blood sugar levels steady and protect your tamaiti’s health. Insulin is usually given by a small needle or pen under the skin, often once or twice a day. The diabetes team will teach you and your whānau how to give these injections safely.
See Starship resources on insulin injections for more information.
See also information to download or read on Ryzodeg
Glucose monitoring
Depending on the type of treatment your tamaiti is on, you may be asked to check their blood glucose levels at home. This is especially important if they are on insulin, as their levels can change more quickly and need closer monitoring. Blood sugar checks are done using a small finger prick to get a drop of blood, which is tested with a glucose meter. The diabetes team will help teach you how to do these checks so you feel confident and comfortable, and they will also prescribe a meter for you to use at home. See Blood Glucose monitoring module for more information.
It’s important to record the glucose readings in a diary, so the diabetes team can see how well the treatment is working and make any needed changes to medicines or doses. See Blood Glucose monitoring module for more information.
Some whānau may be interested in using a Continuous Glucose Monitor (CGM), which shows glucose levels throughout the day and night without as many finger pricks. CGMs are not currently funded for tamariki with Type 2 diabetes in Aotearoa New Zealand. However, some families may be able to use the Carer Support allowance to help with costs. You can read more about financial support options on the KidsHealth New Zealand website
How is Type 2 diabetes diagnosed?
If your tamaiti shows signs of Type 2 diabetes, or has risk factors, a simple fingerprick or urine test may be done to check glucose (sugar) levels. If the glucose level is high, more blood tests might be needed. One of these is called the HbA1c test — this shows how much sugar has been sticking to the red blood cells and gives an idea of what the average blood sugar has been over the past three months.
Other blood and urine tests may also be done to check how well your tamaiti's kidneys and heart are working. This helps plan the best care for your tamaiti.
The medical team will also ask for a special eye test called retinal screening. This is not the usual vision test - it's done by a special team of eye doctors who look at the back of the eye to make sure everything looks healthy and isn't being damaged by high sugar levels.
Finding any changes in the eyes, kidneys, or heart early means we can act early too - and help reduce the chance of long-term problems.
What is Type 2 Diabetes - an overview. Let's go over the main points we've just covered. Ready?
Think you've got it sorted now?
If you have read through the information above and watched the video, and you feel confident that you understand this module, print off and fill in the evaluation form below (you might need to ask someone to print this off for you) and return to the nurse on your ward. If you have any questions, note them down on this form and your diabetes nurse specialist will discuss them with you.
What is type 2 diabetes: Evaluation
After reading this teaching module and watching the Nemours Foundation video, I feel confident that I can understand and describe:
| Yes | No | |
| The causes of Type 2 Diabetes | ||
| Which tests are required to diagnose Type 2 Diabetes | ||
| What are the symptoms of Type 2 Diabetes and why they happen | ||
| How Type 2 Diabetes is treated |
Comments:
Date:
Name:
